MIEP Combines Informatics and Computational Modeling to Study Macrophage Responses to Helicobacter pylori.
BLACKSBURG, Va., Oct. 7, 2015 – Researchers at the Center for Modeling Immunity to Enteric Pathogens (MIEP) at Virginia Tech have completed a comprehensive study on gene networks that regulate macrophage responses to H. pylori, a gut-dwelling bacterium carried by half the world’s population.
Recently published in the open access journal Plos One, the discovery explains how the expression of certain genes changes over the course of an infection in macrophages — information that could lead to early detection or prevention of stomach disorders.
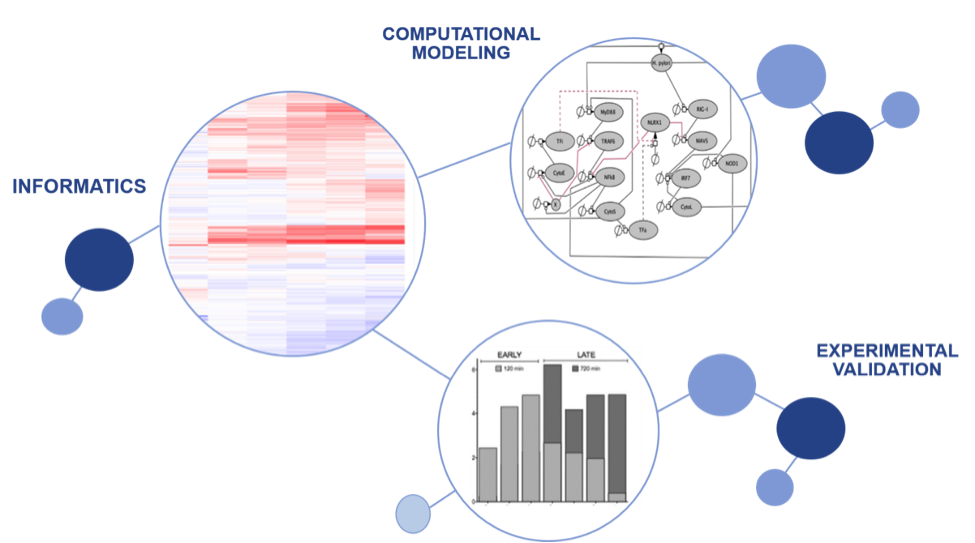
Though H. pylori is most famously associated with peptic ulcers and stomach cancer, its effect on human hosts varies widely depending on the individual. In many cases it even seems to benefit its carriers, contributing to lower instances of obesity and asthma. MIEP researchers are studying how the response of gastric immune cells to the infection affects health outcomes in people who carry this bacterium. To understand the broad spectrum of macrophage responses to H. pylori, the study performed RNA sequencing and identified a set of more than a 1,000 differentially expressed genes at six different periods in the hours following infection in macrophages.
“With this big dataset we were able to see how clusters of innate immune response genes shift during infection,” said Dr. Casandra Philipson, a Nutritional Immunology and Molecular Medicine Laboratory (NIMML) alumna and the Scientific Director of BioTherapeutics. “The temporal behavior of these newly identified gene modules becomes central for determining the impact of H. pylori on the host response. For instance, computational simulations predict that early onset genes control a key checkpoint, namely NLRX1, to balance microbial burden.”
This gene module clustered into 3 novel host response-waves, or temporal patterns, including a newly identified early regulatory element. Upon further characterizing the 3-wave response, the researchers discovered that H. pylori infection is suppressing members in a family of a regulatory NOD-like receptors (NLRs).
Suppression of regulatory molecules, like NLRX1 and NLRC3, has been linked to worsened outcomes in several chronic inflammatory diseases like chronic obstructive pulmonary disease and inflammatory bowel disease (IBD). Down-regulation of these molecules impairs the ability for a host to control the balance between host tolerance and disease during infection.
The significance of this finding is that NLRX1 might be implicated in facilitating the peaceful cooperation between H. pylori and its human host. Loss of NLRX1 significantly reduces H. pylori colonization and results in more hostile immune responses against the bacterium.
Additionally, the researchers characterize for the first time a 3-wave host response to H. pylori infection and use computational simulations as central predicting mechanisms to understand what regulates host-microbial interactions. The main computational hypothesis is that cytokines in the early response wave control the dynamic behavior of NLRX1. This is another novel finding of the study that remains to be validated in upcoming experiments.
“Like many other bacteria that have colonized the human gut for centuries, H. pylori exerts a positive impact on its hosts when managed at a certain level by their immune systems,” said Raquel Hontecillas, the Co-Director of the NIMML. “Our findings about NLRX1 may reveal how this same equilibrium is maintained between humans and many other members of the gut microbiota.”
A multiyear undertaking, the entire research process — from initial genetic sequencing to data analysis, model development to lab tests — was carried out by a diverse team of experts within the Virginia Bioinformatics Institute. This project epitomizes the seamless integration of informatics, data analytics and computational modeling into information processing representations of host-microbial interactions.
“Big data analytics, immunology, computational biology: all of these methods make an important contribution toward answering the big questions of human health,” said Josep Bassaganya-Riera, Director of the NIMML at Virginia Tech. “MIEP’s embrace of team science allows all of that expertise to live under one roof and be applied toward creating computational models of massively interacting systems such as immune responses to infection.”
These discoveries may lead to more accurate, personalized diagnoses about the threats posed by certain bacteria, and provide clues about how to reproduce H. pylori’s occasional health benefits.
This project was supported in part by funding from National Institute of Allergy and Infectious Diseases contract no. HHSN272201000056C
The Virginia Bioinformatics Institute was established in 2000 with an emphasis on informatics of complex interacting systems scaling the microbiome to the entire globe. It helps solve challenges posed to human health, security, and sustainability. Headquartered at the Blacksburg campus, the institute occupies 154,600 square feet in research facilities, including state-of-the-art core laboratory and high-performance computing facilities, as well as research offices in the Virginia Tech Research Center in Arlington, Virginia.
About NIMML
The NIMML Institute is a 501 (c) (3) non-profit public charity foundation focused on a transdisciplinary, team-science approach to precision medicine at the interface of immunology, inflammation, and metabolism. The NIMML Institute team has led numerous large-scale transdisciplinary projects and is dedicated to solving important societal problems by combining the expertise of immunologists, computational biologists, toxicologists, modelers, translational researchers, and molecular biologists. The Institute is headquartered in Blacksburg, VA. For more information, please visit www.nimml.org or contact pio@nimml.org.